Identification of clinical factors associated with poor surgical outcomes in a primary care dataset
Introduction
There are 310 million surgeries worldwide per year, there is a 1-5% short-term mortality and 20% post-surgical complications rate. Aims of the study are to statistically infer clinical factors associated with poor surgical outcomes and to overcome the limitations of missing data.
Data and methods
ResearchOne is a longitudinal, anonymised primary care dataset from TPP. A subsample of 860,649 individual surgeries performed from January 2011 to December 2016 was used. Mortality (1, 3, 6 months), length of survival (LoS), and 12 months increase in electronic frailty index2 (ΔeFI12) were the surgical outcomes using a general linear model with Elastic Net regularisation and iterative fitting along a regularisation path. Confidence intervals were derived via bootstrap sampling (n=150).
Age; sex; use of antihypertensives (AH); eFI at surgery; mean, median, slope, and count of both systolic (SBP) and diastolic (DBP) BP 12 months prior to surgery; socioeconomic status (Index of Multiple Deprivation Ranking 2011); counts of GP visits (GPV) 12 months prior to surgery; and latent variables for missing data were the assumed independent variables. In sensitivity analysis, all missing data were imputed with MICE (n=30) apart from preoperative BP, which was imputed in 39% of cases based on population-level centiles adjusted for age, gender, and AH3.
Key findings
Age, preoperative eFI, and AH were the best predictors for the outcomes ΔeFI12 (95% CI standardised β coefficients (SβC): 0.94-1.06, 0.73-0.86, 0.33-0.37, respectively); and LoS (95% CI SβC: 1.00-1.00, 0.88-0.89, 0.26-0.27, respectively). Low DBP was a predictor for LoS, mortality, and ΔeFI12.
After missing data imputation, no reduction was observed in βC for features with no missing data. However, there was an overall 80% reduction in βC (for all outcomes) for low DBP. In a subsequent analysis, patients with missing BP were found to be a selective subsample: AH, age, eFI, and LoS and ΔeFI12 were predictors of missing BP (95% CI βC: (-1.43, -1.43), (-0.55, -0.54), (-0.42, -0.42), (-0.07, -0.07), (-0.06, -0.06), respectively). The missingness of data was not random and the association between BP and outcomes may be spurious.
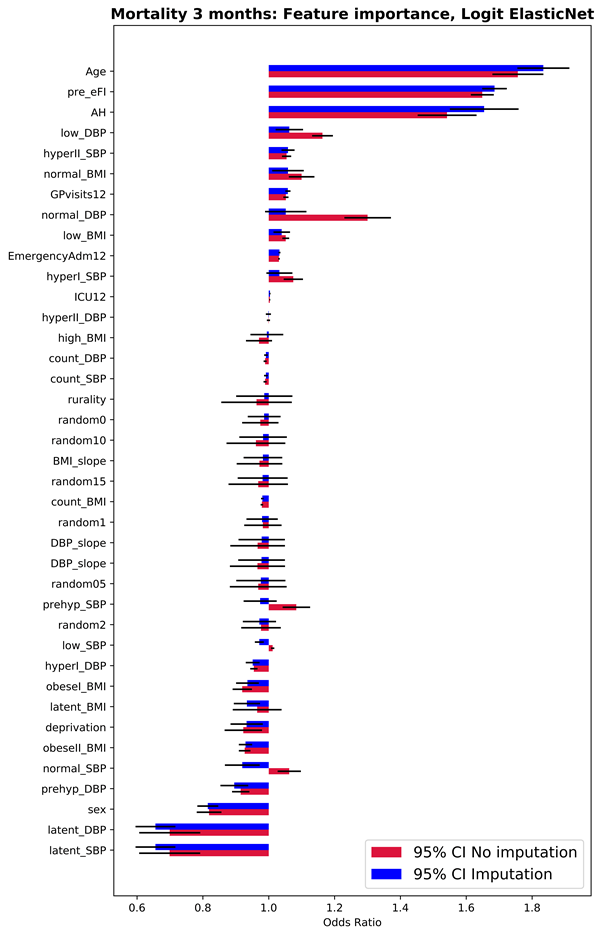
Figure 1 – 95% CI Odds Ratio (OR) for each feature in the prediction of mortality 3 months after using Logit with Elastic Net regularisation and oversampling of the minor class.
Value of the research
While the relationship between postoperative survival and BP requires further clarification, the eFI may warrant further investigation for inclusion in risk assessment measures.
Researchers
David Narganes - Leeds Institute for Data Analytics, University of Leeds
Luke McMenamin and Daniel J. Drayton - Leeds Institute of Biomedical and Clinical Sciences, University of Leeds & Department of Anaesthesia, Leeds Teaching Hospitals
Chris Bates, - TPP
Alywyn Kotze, - Department of Anaesthesia, Leeds Teaching Hospitals
David Wong, - Leeds Institute for Data Analytics, University of Leeds
Simon Howell, - Leeds Institute of Biomedical and Clinical Sciences, University of Leeds; Department of Anaesthesia, Leeds Teaching Hospitals
