Assessing Patient Safety Inequities in Ambulance Non-Conveyance
A 999 call doesn’t always result in hospital transport, as millions of cases are managed without conveyance. This research investigates how socioeconomic and demographic factors influence ambulance non-conveyance decisions, highlighting potential inequities that impact patient safety and healthcare outcomes.
Project overview
Ensuring patient safety within the NHS is a critical priority. Existing research highlights broader safety inequities across healthcare services, with disparities often observed in access, treatment, and outcomes among different patient groups (Marmot et al., 2010). While inequities in ambulance service non-conveyance decisions are less well-documented, initial studies suggest variation in non-conveyance rates influenced by factors such as age, socioeconomic status, and geographic location (O'Hara et al., 2015). However, the extent to which these inequities contribute to adverse patient outcomes, including preventable deaths, remains underexplored. Our work seeks to address this gap by investigating potential safety inequities in ambulance non-conveyance decisions and their impact on patient safety.
Safety incidents result in up to 11,000 deaths each year, adding over £1 billion in treatment costs. Research suggests that addressing these inequities could save 1,000 lives and reduce healthcare costs by £100 million annually (NHS England and NHS Improvement, 2019). Non-conveyance rates vary significantly, ranging from 12% to 51% across emergency cases, imposing substantial costs on healthcare providers, particularly the NHS (Farhat et al., 2023). Therefore, targeted interventions have the potential to improve patient safety, enhance ambulance and ED efficiency, and reduce healthcare costs.
This study explores whether socioeconomic status, health conditions, and geographic disparities influence non-conveyance decisions within the Yorkshire Ambulance Service (YAS). Not all 999 calls result in hospital transport; some patients receive telephone advice, are treated and referred, or are discharged on scene. Using Connected Bradford data, we assess whether certain groups face higher risks of adverse outcomes after non-conveyance, including repeat 999 calls, GP visits, ED visits, ICU admissions, and death within 30 days.
Moreover, by uniquely examining safety inequities in ambulance non-conveyance and leveraging Connected Bradford, patient journeys can be tracked across primary care, emergency services, and hospital admissions. By developing predictive models and data visualisations, we provide data-driven insights to improve policy, paramedic training, and equitable emergency response strategies, addressing disparities in patient safety.
Data and methods
Examining non-conveyance decisions within the Yorkshire Ambulance Service (YAS) is essential for analysing socioeconomic and demographic factors that may contribute to patient safety inequities.
Data for this study were extracted from Connected Bradford, a comprehensive healthcare data warehouse integrating primary care, secondary care, and ambulance service records. Connected Bradford builds upon the Born in Bradford study (Wright et al., 2013) and links patient data using NHS numbers and other identifiers across multiple healthcare settings.
The final dataset after data linkage includes:
- Primary Care Data: GP records for all Bradford-registered patients, including age, sex, ethnicity, and other sociodemographic variables.
- Yorkshire Ambulance Service Data: Electronic patient records detailing conveyance decisions and associated outcomes.
The study focuses on the post-COVID period (2022-2023), analysing Bradford GP-registered patients only. In order to ensure data quality and to mitigate potential biases, duplicate records and multiple instances of the same incident were removed as illustrated in Figure 1.

Figure 1: Flowchart illustrating the data processing steps applied to Yorkshire Ambulance Service (YAS) electronic patient records (EPR) linked within the Connected Bradford dataset (2019–2023).
Using a conveyance indicator, patients were classified as transported or non-transported. Five outcome categories were tracked within 30 days of the initial 999 call:
- Repeat 999 calls
- GP visits
- Emergency Department (ED) visits
- Intensive Care Unit (ICU) admissions
- Death
A data linkage approach was used to track patient trajectories across healthcare settings, allowing a comprehensive assessment of non-conveyance outcomes. Consequently, providing a population-wide perspective, integrating clinical and demographic factors that influence emergency decisions.
Key findings
This study examines patterns of non-conveyance and its impact on patient outcomes, aiming to provide insights into disparities in transport decisions, particularly in cases where patients are not conveyed.

Figure 2: Age distribution showing peaks of conveyed and non-conveyed patients.
The age distribution of conveyed and non-conveyed patients reveals distinct patterns across different groups as shown in Figure 2 above. While both categories primarily consist of older adults, conveyed patients peak between ages 70–85, whereas non-conveyed cases are more evenly spread across age groups. Infants and young children are almost always transported, aligning with emergency protocols that prioritise their medical vulnerability. Middle-aged adults (20–60 years) experience higher rates of non-conveyance, likely due to lower perceived severity and access to alternative healthcare options such as GP visits. Despite elderly patients (60+) being the most frequently transported, a substantial number remain non-conveyed, raising concerns about the underestimation of risk in this vulnerable group. The need for more thorough assessment is highlighted by the fact that 20.78% of non-conveyed patients still required an ED visit within 30 days, and some later required ICU admission or experienced worse health outcomes, including death.
Ethnic disparities are evident in the outcomes of non-conveyed patients (Figure 3). Black and Mixed patients had the highest likelihood of requiring emergency care within 30 days post non-conveyance, with 44% of Black patients (61-80 years) and 50% of Mixed patients (81+ years) visiting the ED. Additionally, Asian patients (61-80 years) had the highest post non-conveyance mortality rate (4%), indicating that some were denied transport despite having serious conditions. 999 recall rates were highest among Mixed (81+ years: 75%) and Black (61-80 years: 44%) patients, suggesting that many still perceived their condition as severe but were initially left without transport. GP visits were more frequent among non-conveyed Black, Asian, and Mixed patients, implying that these groups relied on primary care to manage their conditions after being denied ambulance transport.
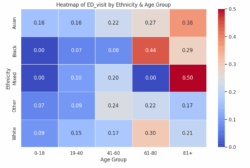
Figure 3: Heatmap of Emergency Department (ED) visits by ethnicity and age in non-conveyance cases.
Overall, these findings highlight the need for a more equitable and risk-sensitive approach to non-conveyance decisions, ensuring that high-risk patients, particularly older adults and ethnic minorities, are not left without critical emergency care. As the next step, logistic regression models will be fitted to quantify the association between sociodemographic variables and conveyance decisions. The focus will be on interpreting the coefficients of key variables, such as ethnicity, age, and deprivation, to determine how they influence the likelihood of being conveyed.
Value of the research
This project raises awareness of the risks associated with non-conveyance, particularly for high-risk groups such as older adults and ethnic minorities. By highlighting delayed emergency care, increased reliance on GP services, and disparities in 30-day outcomes, it provides data-driven insights to improve decision making in ambulance services. The study emphasises the importance of risk sensitive triage protocols, as findings indicate that some non-conveyed patients later required emergency care, ICU admission, or even died. By informing paramedics and healthcare professionals, this research can enhance patient safety, ensuring that vulnerable individuals receive the timely care they need.
Beyond emergency services, the findings have broader implications for healthcare policy and equity. They provide evidence to refine ambulance triage guidelines, develop paramedic training programs, and implement follow-up protocols for high-risk patients. Addressing disparities in transport decisions can contribute to reducing preventable mortality rates and improving long-term patient outcomes. The study also supports resource allocation improvements, helping healthcare providers implement risk-sensitive, patient-centred approaches.
As a result, by providing these findings, emergency services and policymakers can work towards a more equitable healthcare system, ensuring that marginalised groups are not disproportionately affected by non-conveyance decisions.
Quote from project partner
“Inequality and inequity in Patient Safety is a key concern for health service providers and a growing area of research interest. Leveraging the power of system-wide integrated datasets across multiple service areas is an important first step in understanding inequality in patient safety and putting measures in place to address this issue. This initial exploratory work in ambulance service non-conveyance has highlighted what is possible through linkage of Primary, Secondary, Ambulance Service and Sociodemographic Data.”
Safety Intelligence Research Group, Yorkshire & Humber NIHR Patient Safety Research Collaborative.
Insights
- Non-conveyance decisions affect older adults and ethnic minorities more than other groups, increasing their likelihood of requiring emergency care, ICU admission, or experiencing worse health outcomes within 30 days.
- This study uniquely analyses post non-conveyance trajectories, offering a longer-term view of patient risk and healthcare resources utilisation beyond immediate transport decisions.
- Findings can inform ambulance triage protocols, paramedic training, and follow-up care strategies, helping reduce preventable health decline and improve patient safety.
- Research can be expanded to develop decision-support tools for paramedics, assess the impact of non-conveyance follow-up interventions, and further investigate systemic healthcare disparities in emergency response.
Research theme
Health
Programme theme
- The Science of Data Science
- Artificial Intelligence
Team
- Angeliki Fragkeskou, Data Scientist, University of Leeds
- Jonathan Benn, Associate Professor in Healthcare Quality and Safety, School of Psychology, University of Leeds
- Luke Budworth, Senior Research Data Analyst, NIHR Yorkshire & Humber Patient Safety Research Collaboration
Partners
- NIHR Yorkshire and Humber Patient Safety Research Collaboration
- Bradford Teaching Hospitals NHS Foundation Trust
- Connected Bradford
- University of Leeds
- Bradford Institute for Health Research.
Funder
Funded by NIHR Yorkshire and Humber Patient Safety Research Collaboration.
This work has been facilitated by the Leeds Institute for Data Analytics (LIDA) Data Scientist Development Programme, which employs early-career data scientists to deliver real-world data-driven impact in the interests of the public good.
References
Marmot, M., Allen, J., Goldblatt, P., Boyce, T., McNeish, D., Grady, M. and Geddes, I., 2010. Fair society, healthy lives: The Marmot review. London: The Marmot Review.
O'Hara, R., Johnson, M., Hirst, E., Weyman, A., Shaw, D., Mortimer, P., Newman, C., Hird, K. and Siriwardena, A.N., 2015. A qualitative study of systemic influences on paramedic decision making: care transitions and patient safety. Journal of Health Services Research & Policy, 20(1_suppl), pp.45-53.
NHS England and NHS Improvement, 2019. The NHS Patient Safety Strategy: Safer culture, safer systems, safer patients. London: NHS England.
Farhat, H., Aifa, K.E., Alinier, G. and others, 2023. Understanding patient non-transport decision theories in the pre-hospital setting: a narrative review. International Journal of Emergency Medicine, 16, p.69. https://doi.org/10.1186/s12245-023-00528-7
Wright, J., Small, N., Raynor, P., Tuffnell, D., Bhopal, R., Cameron, N., West, J. and others, 2013. Cohort profile: the Born in Bradford multi-ethnic family cohort study. International Journal of Epidemiology, 42(4), pp.978-991.
